My Approach to Therapy
Meeting You Where You Are
My therapeutic approach is intentionally simple, responsive, and deeply person-centred. It’s about meeting you
where you are on the day, not fitting you into a pre-prepared plan. I keep my session notes minimal — often no
more than “held space” — unless there’s something important to record, such as a disclosure or a sudden
change. This means my full attention stays with you, not on paperwork. Minimal notes are not “no notes” — they
are focused, purposeful, and meet professional and safeguarding standards. I also choose not to read referral
notes before we meet. This isn’t because I don’t value other professionals’ insights, but because I want to hear
your story in your words, without the influence of someone else’s opinions or labels. If I need background
information later for your safety or for treatment planning, I will request it then.
Why I Work This Way
I believe therapy is most effective when it is tailored to the individual in the moment. I rarely plan sessions in
advance, though I have a wide range of resources I can draw on. Many of these are created together in the
session — asking you to write down your thoughts, goals, or feelings — so they are truly yours. When you are
actively engaged in the process, change can be powerful. If it becomes clear that a different approach might be
more helpful, I will suggest a referral to another therapist or service, either internally or externally. My priority is
always that you get the kind of support that best meets your needs.
The Ethics Behind My Approach
My way of working is not only intentional, it’s grounded in professional ethical codes and trauma-informed
principles — safety, choice, collaboration, trust, and empowerment. I start with your voice, not someone else’s
notes. By meeting you without reading referral notes first, I reduce the risk of unconscious bias and ensure you
shape the narrative from the start. Minimal notes, maximum presence. I keep records only as needed for safety,
safeguarding, or important changes. This respects your privacy and keeps me present with you. No
one-size-fits-all plans. I respond to what you bring on the day, rather than imposing a predetermined structure.
Your autonomy matters. You are the expert in your own life. I am here to walk alongside you, not lead you down a
path that isn’t yours.
A trauma-informed foundation:
• Safety – You are met without judgement or assumptions.
•Trust – I am transparent about how I work.
• Choice – You decide what to share and how we work.
• Collaboration– We create tools and strategies together.
• Empowerment – Our work builds on your strengths.
For Professionals
If you are a professional or referrer who wishes to understand the ethical reasoning behind my approach, you can
read my full Ethical Position Statement here:
■ Ethical Position Statement (PDF available on request)
This document outlines how my approach aligns with the BACP Ethical Framework, ACCPH Standards, and SAMHSA
Trauma-Informed Care Principles, and why it is both safe and effective.
Full Ethical Position Statement
Purpose
To outline the ethical reasoning behind my therapeutic approach, including minimal note-taking, not requesting
referral notes upfront, and allowing sessions to develop responsively rather than from a fixed plan.
1. Client Autonomy & Self-Determination
BACP Ethical Framework (2018): Counsellors must “respect the right of clients to be self-governing” (Principle:
Autonomy).
My approach ensures the client’s voice is the starting point. I do not seek pre-existing referral notes
before meeting a client, as this protects against unconscious bias and allows their own lived experience to take
priority. This honours the client’s right to shape the narrative about themselves without external interpretation
influencing the therapeutic relationship from the outset.
2. Non-Maleficence & Avoiding Diagnostic Overshadowing
BACP Ethical Framework (2018): Counsellors should “avoid harming clients” (Principle: Non-maleficence).
By avoiding upfront third-party reports, I reduce the risk of prejudgement, misinterpretation, or limiting the client to the language of pathology. This protects the integrity of the therapeutic alliance and prevents harm caused by
imposed labels or deficit-based thinking.
3. Informed Consent & Transparency
BACP Ethical Framework (2018): “Communicate clearly what clients can expect” (Good Practice). My contracting
process explicitly explains that I will start with the client’s own account, keep minimal notes, and co-create
resources as needed. This transparency allows the client to make an informed decision about working with me.
4. Record-Keeping & Safeguarding Compliance
ACCPH Standards & BACP Guidance: Record-keeping must be “appropriate, accurate and timely” and
“necessary for the purpose.” I maintain minimal, focused notes (e.g., “held space”) unless safeguarding,
disclosures, or significant changes require more detail. This ensures confidentiality, reduces unnecessary data
storage, and still meets safeguarding, legal, and professional obligations.
5. Individualised, Needs-Led Practice
BACP Ethical Framework (2018): Counsellors should “be attentive to the needs and best interests of clients.”
I rarely pre-plan sessions and instead meet clients where they are, drawing on resources only when relevant. Many resources are co-created with the client to ensure they are meaningful and empowering. This ensures flexibility, responsiveness, and genuine person-centred practice, rather than a one-size-fits-all model.
6. Trauma-Informed Principles
SAMHSA Trauma-Informed Care Principles: Safety, Trustworthiness, Choice, Collaboration, Empowerment.
•Safety:
Clients are met without judgement or preloaded assumptions. • Trustworthiness: My approach is
transparent from the start.
• Choice:
Clients decide how to share their story and what resources we use.
•Collaboration:
We co-create tools and strategies.
• Empowerment:
The client is the expert in their own life; my role is to walk alongside them.
Summary
This approach is consistent with professional ethical codes, trauma-informed care principles, and the commitment
to do no harm, protect client autonomy, and provide responsive, needs-led support. It is not a refusal to use
existing information or structure, but a conscious sequencing of when and how those elements are introduced to
best serve the client’s interests
Under the Skin: What the Rise of Cosmetic Surgery Says About Self-Worth
You don’t have to look far to see it. Scrolling through social media, watching a reality show, or even chatting with friends, it’s become normal to hear, “I’m just getting a little tweak,” as casually as if they’d said, “I’m getting my hair done.”
Cosmetic procedures — from injectables to full surgeries — have moved from rare, whispered-about luxuries to everyday appointments on the calendar. The message that we should constantly “improve” our appearance has seeped into the mainstream, often so subtly that we forget to question it.
The culture of constant self-editing
We live in a world where filters can erase our lines, apps can slim our shapes, and marketing tells us that beauty is a currency we must protect at all costs. In this environment, it’s not surprising that many feel drawn to make changes that go beyond the temporary.
But here’s the truth: trying to reverse the ageing process doesn’t stop us from growing older. No matter how much we smooth, lift, or tighten, time keeps moving. Our cells keep renewing. Our stories keep unfolding.
Beneath the surface: the inner conversation
As a trauma-informed counsellor, I’ve seen how our sense of self-worth often gets tangled in external expectations. If you’ve grown up in an environment where love felt conditional, where appearance was commented on more than character, or where you learned to measure your value through others’ approval, it’s easy to internalise the belief that “how I look is who I am.”
In those moments, cosmetic surgery can become more than a beauty choice — it can be a coping mechanism. The unspoken hope is, “If I just fix this one thing, I’ll finally feel enough.” But that relief is often short-lived if the deeper wound — the one that whispers we’re not already worthy — hasn’t been acknowledged and healed.
The body as a mirror
Our bodies carry our histories. They reflect not just our age, but our experiences — the joy and the grief, the stress and the love, the moments we laughed until we cried. In a culture that tells us to erase these signs, it’s easy to forget that they’re part of what makes us real.
Changing the outside can sometimes feel like regaining control in a world where so much feels uncertain. But the greatest transformation often comes when we turn inward, building a relationship with ourselves that is based on compassion rather than constant correction.
Compassion over judgement
This isn’t about shaming those who choose cosmetic surgery. We all navigate our bodies and our lives within the same cultural pressures, and for some, a procedure genuinely brings comfort and confidence.
What I’m inviting is curiosity — about why we feel we must change, and whether the change we’re seeking is truly on the surface or somewhere much deeper.
Growing older, growing whole
No surgeon’s scalpel or syringe can pause time. But we can soften the way it moves through us. We can honour the faces we see in the mirror as chapters of our story. And we can invest in the kind of self-worth that doesn’t need perfect lighting to exist.
If we put as much energy into tending our inner world as we do into tending our outer appearance, we might just discover that the beauty we’ve been chasing has been there all along — not under the skin, but at the core of who we are.
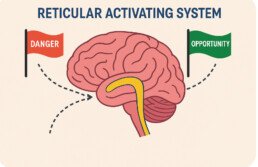
From Danger Detector to Joy Seeker: How the Reticular Activating System Shapes Our Focus
The Reticular Activating System (RAS) is a network in the brainstem that acts like a filter. Every second, it processes millions of bits of sensory data — but it only lets through what matches your current focus or beliefs.
If you’ve ever noticed a certain car model everywhere after thinking about it, or heard your name in a noisy room, that was your RAS at work. It’s like your brain’s personal search engine, prioritising what it thinks matters most.
When you’ve lived through trauma, that filter often becomes tuned to threat detection. Your brain becomes a danger radar — scanning for anything that could confirm “I’m not safe.”
My Story: When the RAS Saved My Life
Years of living in a violent, volatile environment gave my brain a lot of practice spotting danger. I became so finely tuned that I could sense risk before my eyes or ears gave me any obvious clues.
One day, while visiting a house in my professional role, something inside told me to be cautious. I didn’t yet know why. The feeling was almost other-worldly — as if I could sense something my eyes couldn’t yet see. As I approached a room, I realised someone was hiding behind the door — holding a kitchen knife. They were in crisis, believing they were under attack. My awareness meant I could respond calmly, keep my distance, and protect both of us.
This wasn’t the only time these instincts had protected me — it had happened on many occasions. But this was one example that made me stop and really question what was happening in those moments and why my brain seemed to know before I did.
In that moment, my RAS had picked up on subtle cues and changes in the environment before my conscious mind understood them. That skill had been honed over years of living in a dangerous home environment. It had kept me, and those I love, safe.
The Challenge After Danger Passes
Hypervigilance doesn’t switch off the day you find safety. Your RAS keeps scanning for danger, even when danger is no longer there.
Learning to live without that constant alertness takes time. You have to:
- Process what happened and why
- Understand your triggers and reactions
- Learn to tell the difference between real threats and perceived ones
- Practise responding in measured, appropriate ways
It’s hard, and it takes energy. But it’s possible.
Shifting the RAS From Danger to Opportunity
When safety returns, you can begin to retrain your RAS. Instead of searching for threats, you can teach it to notice moments of joy, gratitude, and possibility.
At A Positive Start CIC, we call this shift #seekjoy. The skill you developed in spotting danger doesn’t disappear — it changes purpose. You’re still perceptive and aware, but now your focus is aligned with growth, peace, and opportunity.
This transformation can begin the moment you set your intention toward good. That’s the plot twist we talk about in our Reconnect & Regulate workshop:
Energy flows where focus goes, and neural pathways grow.
How We Use This in Our Work
At A Positive Start CIC, understanding the Reticular Activating System isn’t just theory — it’s woven into everything we do. Every day, we apply it through our TRUST approach: Trigger Recognition, Reassurance, Understanding, Safety, Truth. This is our foundation for creating safety and helping the nervous system switch off its danger signals. We do this through congruence (being real and authentic), compassion, and empathic understanding — the conditions where the RAS can begin to retune from hypervigilance to a healthier balance.
We also weave this knowledge directly into our workshops. In Reconnect & Regulate, we explore the “plot twist” — how the same brain filter that once kept you safe can be trained to notice opportunities, joy, and purpose. In STAND: Parents as Protectors, we help parents understand how their own nervous system responses, shaped by life experience, can influence how they perceive and respond to risk. By building awareness and practical tools, we support both parents and individuals to re-train their RAS to seek safety, connection, and possibility.
Science Explainer: What the RAS Really Does
What It Is:
A network of nerve pathways in the brainstem (part of the reticular formation) that regulates arousal, attention, and the sleep–wake cycle.
Key Functions:
- Filters sensory information and decides what reaches conscious awareness
- Keeps the brain alert to relevant stimuli
- Tunes attention based on repeated focus or strong emotion
Why It Matters:
The RAS strengthens whatever it’s trained to notice. Years of scanning for danger makes danger detection automatic. Repeated focus on safety and opportunity rewires the filter to notice those instead.
References:
- Reticular Formation – StatPearls (NCBI)
- Reticular Formation – Wikipedia
- Reticular Activating System – ScienceDirect
- How the Brain Manages Energy with Selective Focus – Qualia Life
- Neuroanatomy, Reticular Activating System (RAS) – NLM/PMC
- 10 Ways to Activate the Reticular Activating System – Mind Health
- If You Want It, You Might Get It – Medium
📚 Further Reading
- Reticular Formation – StatPearls (NCBI) – Overview of anatomy and function from a trusted medical source.
- Reticular Formation – Wikipedia – Background on the reticular formation and its role in attention.
- Reticular Activating System – ScienceDirect – Topic summaries and research articles.
- How the Brain Manages Energy with Selective Focus – Qualia Life – Practical tips for engaging your RAS.
- Neuroanatomy, Reticular Activating System (RAS) – NLM/PMC – Technical, research-based explanation.
- 10 Ways to Activate the Reticular Activating System – Mind Health – Accessible ways to positively direct the RAS.
- If You Want It, You Might Get It – Medium – An engaging personal take on the RAS.
Final Thoughts…
Your RAS is always listening to what you focus on. The same filter that once kept you alive in danger can become your greatest ally in creating a life you love. When you choose to #seekjoy, you’re not ignoring your past — you’re rewriting the story your brain tells about your future.
Reconnect & Regulate starts again this September- 8 week program, Mondays 6pm -8pm.
Contact us to Reserve Your Seat
https://apositivestart.org.uk/contact/
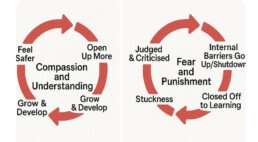
Why Compassion, Empathy and Kindness Are the Foundations of Healing
When we meet someone who is struggling — whether with trauma, neurodivergence, or life’s many challenges — the way we respond matters.
Compassion, empathy, and kindness create safety.
Judgement, criticism, and harshness create fear.
When we feel judged or criticised, our internal defences activate. For people who have experienced complex trauma, these defences often come from a place of survival. They are not a conscious choice — they are an automatic nervous system response.
These reactions can shut us down, block trust, and make moving forward feel impossible.
Self-Compassion: The Bridge Through the Barriers
One of the most powerful tools in healing is self-compassion. It helps us move through shame, fear, and self-criticism. It reminds us that our worth is not dependent on perfection or performance.
Unfortunately, some people mistake compassion for weakness. They believe punishment — or the fear of punishment — is the most effective way to change behaviour. But this is simply not true for everyone. Human beings respond differently. Complex trauma survivors, neurodivergent individuals, and many others often do not respond positively to fear-based approaches.
The Fear of Being ‘Too Kind’
There’s a common worry: “If I’m too kind and compassionate, people will take advantage of me.”
And yes, in the early stages of healing, someone with trauma might push boundaries — not because they are manipulative or disrespectful, but because safety and trust are new to them.
This is where boundaries come in.
We can be compassionate and still be clear. We can be kind and still have limits. The key is to lead by example:
- Stay respectful, supportive, and congruent.
- Communicate in a clear, fair, and honest way.
- Address harmful behaviour without shaming the person.
- Model what healthy boundaries look like.
Regulation Comes First
We can only do this effectively if we ourselves are regulated.
A dysregulated adult cannot help regulate another dysregulated person — whether that’s a child, a partner, a client, or a colleague.
Self-awareness is essential.
Knowing when we are reactive, stressed, or overwhelmed means we can take a step back, regulate, and return with clarity. The difference lies in how we step back — not with hostility, avoidance, or coldness, but with honest communication that maintains connection.
Recognising the Small Steps
Healing is rarely instant.
Every small step counts — and must be recognised.
The more compassion and understanding a person receives, the safer they feel.
For someone experiencing safety for the first time, it can feel like the constant low-level buzzing of anxiety — like the hum of a fridge freezer — suddenly switches off. The panic quietens. The adrenaline eases. The body feels still.
In that stillness, hope emerges — often for the very first time.
The safer we feel, the more open we become.
The more open we become, the more we grow.
And it all begins with compassion, empathy, and understanding.
Based on my own experience of healing — this is what I learned: when compassion is paired with healthy boundaries, safety builds, trust deepens, and transformation follows.
As Carl Rogers put it, healing relationships are built on:
- Congruence – being real and authentic.
- Unconditional Positive Regard – valuing someone for who they are, without conditions.
- Empathic Understanding – truly seeking to understand the other person’s world.
Compassion is not weakness.
It is strength.
It is leadership.
And it is the soil in which healing takes root.
The Distance Travelled
I remember sitting in my home with nothing. No money. No bank account. No reserves.
My abuser had beaten me and squeezed my jaw so hard it was almost broken — all to force me to hand over my benefits. Two weeks’ worth of income for me and my child, gone in an instant.
The electricity had run out on the 50p meter, and I couldn’t afford to top it up. I sat in front of the gas fire, toasting bread and heating a tin of beans for my little one’s lunch. I boiled water on a camping stove for a hot drink — black coffee — because milk was a luxury.
Food was a struggle then. But I tried to make it fun for my child. We played games. Made a den out of duvets and cushions. Pretended we were on a camping trip in the wilderness. The stuffed teddies became elephants, tigers, and bears.
Inside, I was anything but playful. I was trapped in fear. Isolated. Ashamed. Powerless.
This is the hidden reality of domestic abuse. It is not only the bruises and broken bones — it is financial control, isolation, and a slow erosion of your ability to imagine a way out. Many victims are left without access to their own money, stripped of independence, and made to believe they cannot survive on their own. Abusers often manipulate this dependence to maintain control.
And here’s another cruel truth:
Being in this situation rarely brings help.
More often, it draws the wrong kind of attention and the reason many don’t seek outside help.
Victims are judged, scrutinised, and sometimes punished instead of supported.
I have seen mothers lose their children because they found themselves unprepared for a world of abuse — not because they didn’t love or care for them, but because abuse had dismantled their capacity to cope. It is devastating. My own children were the only reason I got up in the morning. They were my sole purpose for living.
Victims do not choose to be abused.
The only person responsible for inflicting suffering is the perpetrator.
And yet, it is so often the victim who is blamed — seen as weak, labelled a failure as a parent. This is a further trauma, one that some never recover from.
I remember waiting. Waiting for something — someone — to notice.
Waiting for someone to come along and change things.
To hand me the solution.
A new place. A job, maybe. A better, kinder life without the fear, the anxiety, and the abuse.
But no one came.
I waited far too long for change to knock on my door.
I waited until it was almost too late — before I realised that the responsibility for change was mine. A victim mentality.
Yes, I had what some call ‘victim mentality’ — because I was a victim. It comes with territory.
It’s a survival mindset, not a weakness. And it doesn’t just vanish the moment you escape harm.
When you’ve been living in fear, your nervous system has learned to scan constantly for danger. That doesn’t stop overnight. In fact, without the right support, you can feel like you’re drifting alone in open water — no raft, no land in sight.
That’s where co‑regulation becomes so vital.
It’s the steady presence of someone regulated enough to hold space for you, so your nervous system can begin to believe it’s safe. This is why our TRUST Framework exists — to provide a foundation of safety, connection, and predictability while survivors learn to navigate life after harm.
It might sound ridiculous now, but I truly had no concept that a person could harm someone so severely and no one would step in to stop it. Late teens, timid and naive, I was still a child myself in many ways. This is the cruelty of abuse — it warps your perception of what’s possible, making you believe you are powerless.
Powerlessness is often an illusion — but when you’re living in survival mode, it doesn’t feel like that.
When you’re in a state of dorsal collapse, everything feels broken, pointless, and empty. It’s not a reflection of who you are, but the only lens you can see through in that moment. The world looks unchangeable because your nervous system is trying to keep you safe by shutting you down.
But when that perception shifts — even slightly — the illusion of powerlessness can begin to fade. Moving your nervous system from dorsal collapse into a more activated survival state, such as fight or, in my case, flight, changes the view. You start to see glimmers of possibility. In fight mode, you can push back. In run mode, you can move towards something better.
And with time, safety, and healing, you can find yourself in a ventral state — the place where your nervous system feels regulated and safe. From here, the lens changes completely. You can see options, hope, and a future that once felt impossible
Understanding the dorsal state is vital for suicide prevention.
When someone is deeply shut down, it can look from the outside like they’re “quiet” or “coping” — but inside, it can feel like there’s no way out. This is when hopelessness can take hold. It’s not that the person truly wants to die — it’s that their nervous system is locked in a state where they can’t see a future worth living. Recognising the signs of dorsal collapse, and helping someone shift — even slightly — into a more mobilised state, can be life-saving. It can help them see through a different lens, one where possibilities and reasons to keep going become visible again.
The day I realised that no one was coming to save me — that the only person who could save me was me — was the day everything began to change.
My life was a mess, but I made a choice:
I escaped.
I studied.
I learned.
I became my own project — unpicking what was wrong, understanding what was happening inside me, and finding ways to heal. I learned about trauma, the nervous system, the cycle of abuse, and the way fear rewires the brain.
And today, when I look at the distance travelled…
When I see what I’ve survived…
When I see my children safe, healthy, and happy…
When I see myself helping others find a way out of their pain and suffering…
I can finally look back at the journey with compassion and kindness for the woman I was.
To anyone still living in fear: I know how it feels to wait for rescue. But I also know the power that comes when you realise that you can be your own rescuer.
I tell myself what I so often tell others:
Look at who you are. Look at what you survived. Look how far you’ve come. You are unstoppable.
“Every journey to freedom begins with a single brave step — your positive start.”
The Illusion of Inclusion: When Trauma-Informed Practice Misses the Mark
In recent years, the phrase “trauma-informed” has become widespread across services—from schools to healthcare to local authorities. On paper, this is a welcome shift. It signals a growing awareness that trauma shapes behaviour, that safety matters, and that healing requires more than just surface-level support.
But for those of us with lived experience of trauma—especially those working in grassroots, community-based organisations—the reality often tells a different story.
Behind closed doors, beneath the polished language, many of us encounter something we don’t talk about enough: exclusion by stealth.
It rarely looks like open hostility. It’s more subtle than that. A non-response to a genuine offer of support. A delay that quietly becomes a dead-end. A vague deferral to someone higher up. An event ignored. A training opportunity dismissed—not on merit, but on the assumption that grassroots must mean lesser.
What sits underneath this pattern is something we know well from trauma itself: power and control.
When institutions hold power, they often expect grassroots organisations to seek their approval. Even when the work is impactful, life-changing, or beautifully person-centred—if it hasn’t passed through the right hierarchy, it is often minimised or dismissed. This isn’t just disappointing. It’s damaging.
What’s most concerning is that these same organisations frequently brand themselves as trauma-informed.
But here’s the truth: You cannot be trauma-informed and still ignore, belittle, or exclude people doing this work from a place of lived experience and heart.
You cannot claim to value relational safety while practising selective inclusion.
You cannot promote emotional wellbeing while perpetuating systems of silence, dismissal, and quiet judgment toward those who don’t fit the mould.
And you cannot truly serve people affected by trauma if you continue to replicate the very dynamics that caused the harm in the first place: gaslighting, blame-shifting, disconnection from impact.
Criticism disguised as concern. Collaboration refused without explanation. Feedback filtered only through formal structures. These are not neutral actions. They are indicators—signs that something is out of alignment, no matter how well-branded the service may be.
From the lens of trauma, they speak volumes.
Lived experience teaches us to listen beyond words. To sense when safety is performative, when empathy is selective, when partnerships are conditional. This isn’t bitterness—it’s discernment.
And it’s time we named it.
Because being trauma-informed is not about a course completed or a policy drafted. It is about how people feel in your presence. It is about humility. Curiosity. Willingness to share space and power. And it is about recognising that those closest to the pain are often also closest to the solutions.
Grassroots organisations are not asking for special treatment. They’re asking to be treated with the same dignity, respect, and openness that trauma-informed services promise to extend to the people they serve.
To those who claim trauma-informed values while gatekeeping lived experience and excluding community efforts—we invite reflection. Not defensiveness. Not justification. But reflection.
Because if your trauma-informed approach does not include the voices, work, and wisdom of those walking the path with survivors every day—then something vital is missing.
A truly trauma-informed response isn’t about doing more than you can manage. It’s not about stretching your capacity or saying yes to everything. It’s about being honest, respectful, and clear. When someone offers training, collaboration, or extends an invitation—what matters most isn’t whether you say yes, but how you say no. Not replying at all, ignoring RSVPs, or disappearing into silence may feel like the path of least resistance, but for those with trauma histories, it echoes something familiar: being disregarded, invalidated, or avoided.
Trauma-informed practice craves truth. It thrives on transparency, even if the message is “I’m too busy,” “It’s not the right fit,” or even “We’re not interested at this time.” That’s okay. Clarity is not cruelty. But avoidance? That’s often where harm begins.
In the trauma-informed world, we teach that it’s not about perfection—it’s about presence. And sometimes the most compassionate thing a professional can do is respond with integrity, even when the answer is no.
Because in the end, it’s not the survivor who fears the truth—it’s often the system.
This isn’t a new observation. We’ve been speaking about it for a while now—and we know we’re not alone.
Other grassroots organisations have shared the same experience: being overlooked, dismissed, or quietly copied by larger charities and commissioned services. Original ideas are lifted, rebranded, and re-released without so much as a nod of acknowledgement. Meanwhile, those of us on the ground—often running on passion, purpose, and very little funding—are told we don’t have the “track record” to access support or scale our work.
It’s a disheartening cycle: grassroots organisations are excluded because they’re not funded, and they’re not funded because they’re excluded.
But every now and then, something feels different. Working with My Body is My Body (MBIMB) has been just that. A refreshing reminder that collaboration can be equal, respectful, and joyful. There’s no sense of hierarchy, no guardedness or gatekeeping—just genuine partnership rooted in shared values and mutual respect.
The difference is palpable. And it’s proof that safe, trauma-informed relationships are possible when ego is set aside and hearts lead the way.
This is exactly why My Body is My Body is a global initiative—because it puts people first.
It’s led with heart, rooted in equality, and carried by those who understand the difference between performative inclusion and real connection. It models what trauma-informed practice should feel like: safe, respectful, empowering, and true.
This kind of heart-led collaboration is the future. It’s what genuinely trauma-informed systems should look and feel like—equal, respectful, and rooted in shared purpose. We welcome it, we celebrate it, and we’re committed to creating more of it.
Time-Limited Therapy and the Myth of Quick Healing
Time limits make sense in many areas of life. But not in healing. Not in therapy. And certainly not when we’re working with complex trauma.
Too often, I meet people who have been offered six or eight sessions of therapy — sometimes as little as a single hour per week — and then expected to “pick up the reins” and carry on. Alone.
We know why this happens. Funding. Staffing. Systems under pressure. It’s not that individual professionals don’t care — many do. But when services are shaped by cost rather than compassion, the result is always the same: the person gets squeezed into a model that doesn’t fit them.
And those time limits send a message.
“Try harder.”
“Heal faster.”
“You should be better by now.”
This pressure is the opposite of what trauma survivors need.
For those living with the effects of complex trauma — long-term abuse, neglect, fear, loss, shame — healing is not linear, and it’s never quick. The nervous system doesn’t respond to pressure by settling. It responds by shutting down or speeding up. Neither of which supports reflection, insight, or regulation.
And beneath all of this, it taps into something even deeper — the early, unspoken beliefs many trauma survivors carry: I’m not good enough. I’m too slow. I’m not trying hard enough. These beliefs were often formed in childhood, in environments where love was conditional, safety was unpredictable, and performance was the only path to approval. When therapy is limited by time and framed around progress, it risks reinforcing these very wounds. The healing space becomes another place where the old story plays out: You’re too much. You’re not enough. Hurry up and get better. This doesn’t just stall healing — it perpetuates the cycle.
And yet, I’ve heard therapists justify time limits with phrases like, “We don’t want clients to become dependent on therapy.”
Curiously, the same concern doesn’t seem to apply to medication.
Many of the people I work with have been prescribed anti-anxiety medication or antidepressants for decades — often with no review, no therapeutic input, and no alternative offered. There is no rush there. No cut-off date. No limit placed on pharmaceutical dependence.
But offer the same person the chance to talk, to build trust, to process their experiences in relationship with another human being — and suddenly we’re watching the clock.
You can’t fast-track trust.
Eight sessions — that’s eight hours — is barely time to build any relationship, let alone a therapeutic one. Especially for people who feel about as far removed from safety and connection as it’s possible to be.
True healing happens in safe spaces, over time, in relationships that are steady, honest, and consistent.
Being trauma-informed means we meet people where they are. We honour their pace. We don’t pressure them to change on a schedule. We create space for safety, for understanding, for feeling — and for silence, too.
Because healing can’t be rushed. It never could be. And it never will be.
When Love and Empathy Are Misunderstood
Too Soft? Too Compassionate? Good.
When Love and Empathy Are Misunderstood – A Call for Something REAL
There’s a particular kind of pain that comes with seeing someone in trauma—whether a child, a parent, or a student—when no one else seems to see it.
They see a troublemaker, a problem, a drain.
You see a child frozen in shame, or flailing in fear.
You see connection-seeking—not attention-seeking.
You recognise the signs. The nervous system shutdowns. The survivor strategies. The dorsal vagal collapse hiding behind the outbursts or silences.
And when you name it?
You’re dismissed.
“You’re too soft.”
“You’re enabling them.”
“You’re being manipulated.”
“Stop mollycoddling them.”
When you’ve lived through trauma, you understand these patterns. You don’t just know them intellectually—you feel them. And it’s that felt sense that guides how you show up: with compassion, with care, and sometimes with a quiet rage when you’re forced to watch harm unfold and can do nothing to stop it.
The Moral Injury of Being Trauma-Informed in a System That Isn’t
The term moral injury describes the psychological and emotional toll of witnessing (or participating in) something that violates your deepest values. It’s not burnout. It’s not compassion fatigue. It’s the soul-splintering ache of knowing better and being unable to do better because the system won’t allow it.
I experienced this deeply in my role as a school counsellor—a position I loved. I cared for the children, saw their stories behind their behaviour, and held hope for their healing. But I also saw how the system responded: punishment instead of curiosity, control instead of connection.
Over time, it kept me awake at night.
Eventually, I had to walk away—not from the children, but from a system I could no longer stomach. I chose to support from outside, because staying meant betraying myself. And what use is a trauma-informed counsellor if she’s constantly overriding her own nervous system just to survive the working day?
Some days, the grief still visits.
Other days, I wonder: When these systems finally catch up… what then?
What happens when people realise how many children were harmed unnecessarily? How many were labelled instead of loved? Punished instead of protected?
Will we see litigation ads in 10 years—“If you or your child were harmed by a punitive education or care system, you may be entitled to compensation…”?
It sounds absurd now, but so did asbestos claims. So did tobacco lawsuits. So did the idea that trauma lived in the body. And now, here we are.
A Vision for the Future
I dream of a world where kindness, compassion, and trauma-informed care are not just tolerated but expected. Where the TRUST and philosophy frameworks are common knowledge—not quirky ideas from a fringe outsider like me.
Where systems put people before profit, and survival responses are met with understanding—not control.
Where we stop asking, “What’s wrong with you?” and start asking, “What happened to you?”
And most importantly, where those who care deeply are no longer labelled as soft or weak—but recognised as essential.
Let’s Build Something REAL
In response to this growing disconnect, I’ve created a space called REAL:
A WhatsApp community for trauma-informed professionals and practitioners who have experienced moral injury, dismissal, and the isolation that comes with seeing what others won’t see.
REAL stands for:
🔹 Regulated
🔹 Ethical
🔹 Accessible
🔹 Lived experience-led
No egos. No selling. No pretense. Just genuine connection, shared experiences, and support for those of us who feel like we’re shouting into a void—or have walked away because we just couldn’t take it anymore.
If this resonates, you’re not alone. And you’re not the problem.
You’re the future.
Here’s the link if you’d like to join the REAL group—or just want to talk
https://chat.whatsapp.com/B4tqnF62qpf8F8ZDrSxnlJ?mode=ac_t
#TraumaInformed #MoralInjury #CompassionIsStrength #EducationReform #PeopleBeforeProfit #LivedExperience #REALSupport #EmpathyMatters #PositiveChange
The Cost of Incongruence in Trauma-Informed Practice
It’s easy to say the right things.
“Inclusive.”
“Person-centred.”
“Trauma-informed.”
These words are everywhere—in training manuals, policies, funding bids, and introductory slides.
But saying the right thing isn’t the same as living it.
When someone raises a concern, gives feedback, or reaches out with lived experience, the responses often sound like this:
“We’re really busy.”
“We’re doing our best.”
“You misunderstood.”
“You should have followed up.”
“You could have done more.”
That last one is particularly revealing.
It subtly shifts the responsibility back onto the person who had already made the effort. It reframes a lack of response as a lack of effort—on their part.
But when you claim to be inclusive or trauma-informed, the burden doesn’t fall on the most vulnerable to keep pushing for your attention.
Inclusion doesn’t mean “chase me.” It means “we see you.”
Incongruence Is a Safety Issue
For trauma survivors, inconsistency between words and actions isn’t just disappointing—it can be deeply destabilising.
It mirrors earlier experiences where people said all the right things but failed to follow through. Where safety was promised but not delivered. Where connection was conditional, performative, or superficial.
This kind of relational rupture—especially from services or professionals claiming to be trauma-informed—can reinforce beliefs like:
- “People don’t mean what they say.”
- “I was right not to trust.”
- “It’s not safe to ask for help.”
These aren’t just thoughts. They are nervous system responses. They shape the way people relate to others—and to themselves.
It’s pointless doing the worksheet, if the learning isn’t applied!
Being trauma-informed isn’t about printing posters, doing a one-off CPD session, or including buzzwords in reports.
It’s about:
- Reflection: How does what I do impact those I support?
- Responsiveness: Am I open to feedback, or am I defending my image?
- Repair: When something goes wrong, do I show up or shut down?
If your trauma-informed practice begins and ends with paperwork, it isn’t trauma-informed. It’s performance.
Calling out the mismatch between words and actions is never easy—especially for those with lived experience of trauma. It takes courage to speak up when something doesn’t feel aligned.
But instead of responding with reflection, the default is often defence.
Rather than examine the gap, the system closes ranks.
And the person who spoke up becomes the problem.
“She’s difficult.”
“She’s too intense.”
“She’s being unprofessional.”
“She’s arrogant.”
“She’s always got an issue with something.”
These aren’t objective reflections—they’re projections.
They come from discomfort. From a need to protect image over integrity. From an inability—or unwillingness—to sit with the truth that something might need to change.
This is a subtle form of victim blaming.
It puts the emotional cost back on the person holding up the mirror.
And when that person is a trauma survivor, it reinforces every old story about being “too much,” “not worth it,” or “hard to love.”
The irony is painful: the very practices that claim to protect people end up pathologising them when they speak truth to power.
Doing the worksheet and putting it back in the drawer isn’t enough.
If you’re not adapting, developing, and growing—it’s just lip service.
Say What You Mean. Mean What You Say!.
Being person-centred means responding to the person—not just their file.
Being inclusive means making space even when it’s uncomfortable.
Being trauma-informed means being willing to look inward, not just outward.
It’s not about perfection. It’s about congruence.
Because when actions don’t match words, it doesn’t just erode trust—it can deepen harm.
So in a world full of statements, be someone of substance.
Say what you mean. Mean what you say.
And if you fall short—repair, don’t retreat.
‘We Borrow Health from Tomorrow’ – Exercise, Diet & Trauma Recovery in Midlife
When we’re young, we rarely think twice about what we eat, how much we move, or whether we’re getting enough rest. Our bodies seem to just get on with it. Late nights, takeaways, skipping meals, or grabbing sugar and caffeine to keep going—somehow, we bounce back.
But what we don’t realise is that in those younger years, we’re borrowing health from tomorrow.
And eventually, tomorrow comes.
As we move into midlife—often around the same time trauma and unresolved emotional patterns begin to show themselves more vividly—we start to feel the consequences. The body keeps the score, as Bessel van der Kolk reminds us, and it also sends the bill.
What Starts to Show Up
And for women, menopause adds another layer. Hormonal shifts during perimenopause and menopause can amplify the effects of poor diet and stress.
Trauma & the Nervous System
For those of us with trauma histories—especially complex or developmental trauma—the nervous system has often been running on survival mode for decades. This means our bodies have been prioritising immediate safety over long-term health. Digestion, immune function, hormone balance, and rest become secondary when we’re stuck in a sympathetic (fight/flight) or dorsal vagal (shutdown) state.
The Hidden Cost of Stress & Adverse Childhood Experiences (ACEs)
Stress—especially chronic stress rooted in unresolved trauma or adverse childhood experiences (ACEs)—has a profound effect on the body. The nervous system, designed to keep us safe, can become stuck in survival states, constantly scanning for danger. Over time, this prolonged state of hypervigilance impacts digestion, hormone regulation, immune function, and sleep quality. It’s no wonder many of us feel exhausted, inflamed, and overwhelmed by midlife.
In the absence of safety, food often becomes a coping mechanism. We reach for sugar to self-soothe, caffeine to stay alert, and carbohydrates to feel comforted. Emotional eating is not a character flaw—it’s a survival strategy. But while it may bring short-term relief, it often leads to long-term imbalance. Recognising this pattern with compassion is the first step toward healing. Nourishing the body with steady, grounding meals can help restore a sense of safety and support emotional regulation.
Healing from trauma is deeply connected to how we care for the body. It’s not just about therapy—it’s about nourishment, movement, hydration, sleep, and compassion.
You Can’t Put an Old Head on Young Shoulders…
It’s true. Until something becomes real, personal, and felt in the body, it’s hard to act. We don’t know what we don’t know. But if we want the next generation to avoid the pain and confusion many of us face in midlife, we must educate early and lead by example—not with fear, but with knowledge, curiosity, and compassion.
What Does a Healthy, Balanced Diet Look Like?
A balanced diet isn’t about perfection or punishment. It’s about giving the body what it truly needs to function well and heal.
It’s Never Too Late to Begin
Making changes in midlife can feel overwhelming, especially when trauma has made food a source of comfort or control. But this is also a powerful time. With the right support, you can begin to restore the relationship between your body, your choices, and your healing.
Start small. Walk daily. Add one more vegetable to your plate. Drink water when you feel foggy. Swap out sugary snacks for protein-rich alternatives. Pause before pouring another coffee.
Every small choice is a signal to your body: I’m listening now.
Let’s Break the Cycle for the Next Generation!
We didn’t know what we didn’t know. But we do now. Let’s use that wisdom to break generational patterns. Let’s show our children that nourishment is an act of self-respect, not restriction. That movement is medicine, not punishment. That healing includes the body as much as the mind.
Because a positive start… starts with us!